In the vast sea of biomarkers and lipid profiles that can predict cardiovascular disease (CVD), a relatively lesser-known yet critical player stands out: Lipoprotein(a) or Lp(a). This comprehensive guide covers the importance of Lp(a) and its link to cardiovascular health. You’ll also learn the best methods to manage Lp(a) and LDL cholesterol.
What is Lp(a)?
Lipoprotein (a) is a complex molecule made up of two different parts: LDL (low-density lipoprotein) and a protein called apolipoprotein (a). You may be familiar with the former, as LDL cholesterol deposits can often damage the delicate inner lining of the arteries, opening up an opportunity for plaque buildup. LDL cholesterol is usually dubbed “bad cholesterol” because it can eventually cause a narrowing of the arteries or atherosclerosis.
The production and structure of Lp(a) are largely genetically determined and can vary significantly among individuals. High levels of Lp(a) are considered a significant risk factor for CVD or a cardiovascular event. This is attributed to its atherogenic and inflammatory properties and thrombogenicity, which contribute to the formation of fatty plaques in the arteries and can lead to abnormal blood clotting.
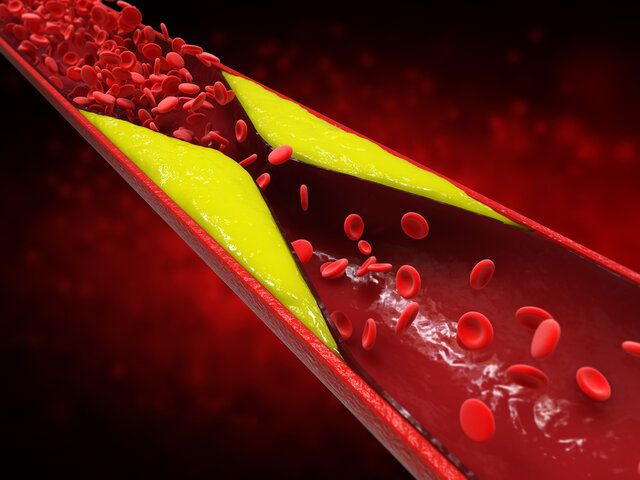
Lipoprotein particles(a) and LDL particles can cause plaque buildup on arterial walls.
How to Screen for Lp(a) Levels
Healthcare professionals screen for Lp(a) levels through a blood test, like other lipids, including HDL and LDL cholesterol levels, triglycerides, and very low-density lipoproteins. The test measures the Lp(a) amount in your blood, typically using an enzyme-linked immunosorbent assay (ELISA).
It’s important to note that because Lp(a) levels are primarily determined by genetics, they do not significantly fluctuate with short-term changes in diet or other factors.
Risk Factors That Increase Lp(a)
- Familial Hypercholesterolemia
- Chronic Kidney Disease and Nephrotic Syndrome
- Menopause
- Hypothyroidism
Interpreting Your Lp(a) Test Results
Understanding the results of an Lp(a) test can help you and your healthcare provider determine your risk for developing CVD. Generally, Lp(a) levels over 50 milligrams per deciliter (mg/dL) are considered high, and levels over 100 mg/dL are considered very high. High Lp(a) levels, especially in combination with other risk factors like high LDL cholesterol, low HDL cholesterol, and a family history of cardiovascular disease, may prompt more aggressive management strategies to prevent or treat heart disease.
Your doctor may suspect that you have high Lp(a) if you have:
- History of early heart attack (before the age of 55 in men or 65 in women)
- Family members that have had early heart attacks or strokes
- Familial hypercholesterolemia
- Aortic stenosis

A doctor can monitor those with familial hypercholesterolemia and help keep Lp(a) and LDL levels low.
Decreasing Lp(a) Levels with Lifestyle Changes
While you can’t change your genetic makeup, there are lifestyle modifications that can help lower high Lp(a) levels and reduce your overall risk of heart disease. These changes include:
- Regular Exercise. Physical activity is associated with lower Lp(a) levels and higher HDL particles. HDL cholesterol can aid in transporting excess cholesterol back to the liver for processing. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Healthy Diet. A diet rich in fruits, vegetables, whole grains, lean proteins, and low in saturated fat can help manage Lp(a) and other lipid levels. Diets low in sugar can also help manage triglyceride levels.
- Maintain a Healthy Weight. Obesity is linked to higher Lp(a) levels, so maintaining a healthy weight is vital.
- Stress Management. Chronic stress can impact LDL particles, including Lp(a) levels. Techniques such as meditation and mindfulness can help manage stress.
- Quit Smoking. Smoking can raise Lp(a) levels and lead to an increased risk for a cardiovascular event, so quitting is an integral part of any effort to lower CVD risk.

A healthy diet low in saturated fats and fiber can help manage Lp(a), high cholesterol, and triglyceride levels.
Supplements for Managing Lp(a) Levels
Several supplements have shown promise in managing Lp(a) levels and lipoprotein metabolism. These include:
- Niacin(Vitamin B3). Niacin is a B vitamin that can modestly lower Lp(a) levels and is sometimes used in addition to statin therapy.
- L-lysine. An essential amino acid, L-lysine has been studied for its possible role in reducing Lp(a) levels. If combined with vitamin C and L-proline, this cocktail can help improve and protect the function of blood vessels.
- Omega-3 Fatty Acids. In fish oil supplements, omega-3s can help lower triglycerides, which can be elevated in those with high Lp(a) levels.
- Coenzyme Q10(CoQ10). This nutrient is highly concentrated in the heart tissue and is involved in energy production. Some studies suggest promising results when taken with statins.
It’s important to note that while these supplements may help, they should only be taken under the guidance of a healthcare professional. They can interact with other medications and have side effects.
Medication for High Lp(a) Levels
If lifestyle changes and supplements fail to lower your Lp(a) levels, your doctor may prescribe medications specifically designed to lower Lp(a) and LDL cholesterol. These include:
- Niacin. As mentioned earlier, niacin can be effective in some individuals, especially in combination with other cholesterol medications.
- Proprotein Convertase Subtilisin/Kexin Type 9(PCSK9) Inhibitors. These newer medications can lower Lp(a) levels substantially and are typically used in those with very high Lp(a), familial hypercholesterolemia, and a history of CVD.
- ApoB Antisense Oligonucleotide Therapy. A new class of drugs, these have shown significant promise in reducing Lp(a) levels and are currently being investigated.
Working closely with your healthcare provider to monitor these medications’ effects and weigh the benefits against the risks and costs is essential.

Many cholesterol medications work at a cellular level and protect blood vessels from plaque buildup.
The Future for Lp(a) and Heart Health
Research into Lp(a) continues to evolve, with new therapies and management strategies being developed. There is also a growing interest in Lp(a) as a target for new cardiovascular therapies, such as RNA-based interventions that could translate into more effective ways to lower cholesterol levels and manage the risk of CVD.
Have You Tested Your Lp(a) Levels Yet?
Understanding and managing your Lp(a) levels can be critical to heart health. You are taking proactive steps toward a healthier heart by staying informed, making lifestyle changes, considering supplements, and working with your doctor to explore medication options. The first step to taking control of your cardiovascular health is to get Lp(a) and other cholesterol particles tested. Remember, the key to optimal heart health is a comprehensive approach that addresses all the potential risk factors, and Lp(a) is an integral part of that equation.
For more information on our upcoming studies, visit our Current Studies page or call us at (954) 582-7007.
Read more: Distinguishing Between Fibroids and Endometriosis: A Comparative Analysis

